What is heart failure?
The term "heart failure" can be frightening. It doesn't mean the heart has "failed" or stopped working. It means the heart doesn't pump as well as it should.
Heart failure is a major health problem in the United States, affecting about 5.7 million Americans. About 550,000 new cases of heart failure occur each year. It's the leading cause of hospitalization in people older than 65.
If you have heart failure, you'll enjoy better health and quality of life if you take care of yourself and keep yourself in balance. It's important to learn about heart failure, how to keep in good balance, and when to call the doctor.
How common is heart failure?
Almost 6 million Americans have heart failure, and more than 870,000 people are diagnosed with heart failure each year. The condition is the leading cause of hospitalization in people over age 65.
Heart failure and aging
Although the risk of heart failure does not change as you get older, you are more likely to have heart failure when you are older.
Women and heart failure
Women are just as likely as men to develop heart failure, but there are some differences:
- Women tend to develop heart failure later in life compared with men.
- Women tend to have heart failure caused by high blood pressure and have a normal EF (ejection fraction; see below).
- Women may have more shortness of breath than men do. There are no differences in treatment for men and women with heart failure.
What are the types of heart failure?
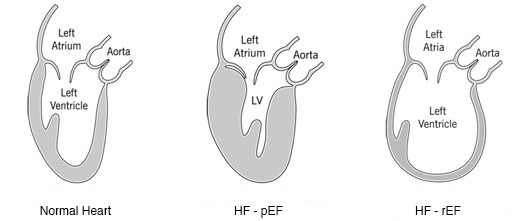
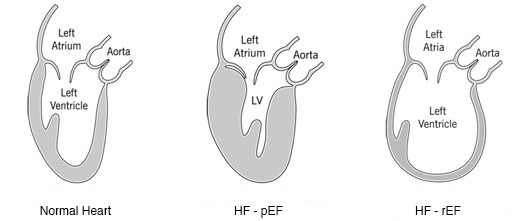
There are many causes of heart failure, but the condition is generally broken down into two types:
Heart failure with reduced left ventricular function (HF-rEF)
The lower left chamber of the heart (left ventricle) gets bigger (enlarges) and cannot squeeze (contract) hard enough to pump the right amount of oxygen-rich blood to the rest of the body.
The lower left chamber of the heart (left ventricle) gets bigger (enlarges) and cannot squeeze (contract) hard enough to pump the right amount of oxygen-rich blood to the rest of the body.
Heart failure with preserved left ventricular function (HF-pEF)
The heart contracts and pumps normally, but the bottom chambers of the heart (ventricles) are thicker and stiffer than normal. Because of this, the ventricles can't relax properly and fill up all the way. Because there's less blood in the ventricles, less blood is pumped out to the rest of the body when the heart contracts.
The heart contracts and pumps normally, but the bottom chambers of the heart (ventricles) are thicker and stiffer than normal. Because of this, the ventricles can't relax properly and fill up all the way. Because there's less blood in the ventricles, less blood is pumped out to the rest of the body when the heart contracts.
What is ejection fraction?
Ejection fraction (EF) refers to how well your left ventricle (or right ventricle) pumps blood with each heart beat. Most times, EF refers to the amount of blood being pumped out of the left ventricle each time it contracts. The left ventricle is the heart's main pumping chamber.
Your EF is expressed as a percentage. An EF that is below normal can be a sign of heart failure. If you have heart failure and a lower-than-normal (reduced) EF (HF-rEF), your EF helps your doctor know how severe your condition is.
How is EF measured?
Ejection fraction can be measured using:
- Echocardiogram (echo) - this is the most common way to check your EF.
- Magnetic resonance imaging (MRI) scan of the heart.
- Nuclear medicine scan (multiple gated acquisition MUGA) of the heart; also called a nuclear stress test.
Why it’s important to know your EF
If you have a heart condition, it is important for you and your doctor to know your EF. Your EF can help your doctor determine the best course of treatment for you. Measuring your EF also helps your healthcare team check how well our treatment is working.
Ask your doctor how often you should have your EF checked. In general, you should have your EF measured when you are first diagnosed with a heart condition, and as needed when your condition changes.
What do the numbers mean?
Ejection Fraction (EF) 55% to 70%
- Pumping Ability of the Heart: Normal.
- Level of Heart Failure/Effect on Pumping: Heart function may be normal or you may have heart failure with preserved EF (HF-pEF).
Ejection Fraction (EF) 40% to 54%
- Pumping Ability of the Heart: Slightly below normal.
- Level of Heart Failure/Effect on Pumping: Less blood is available so less blood is ejected from the ventricles. There is a lower-than-normal amount of oxygen-rich blood available to the rest of the body. You may not have symptoms.
Ejection Fraction (EF) 35% to 39%
- Pumping Ability of the Heart: Moderately below normal.
- Level of Heart Failure/Effect on Pumping: Mild heart failure with reduced EF (HF-rEF).
Ejection Fraction (EF) Less than 35%
- Pumping Ability of the Heart: Severely below normal.
- Level of Heart Failure/Effect on Pumping: Moderate-to-severe HF-rEF. Severe HF-rEF increases risk of life-threatening heartbeats and cardiac dyssynchrony/desynchronization (right and left ventricles do not pump in unison).
Normal Heart. A normal left ventricular ejection fraction (LVEF) ranges from 55% to 70%. An LVEF of 65%, for example means that 65% of total amount of blood in the left ventricle is pumped out with each heartbeat. Your EF can go up and down, based on your heart condition and how well your treatment works.
HF-pEF. If you have HF-pEF, your EF is in the normal range because your left ventricle is still pumping properly. Your doctor will measure your EF and may check your heart valves and muscle stiffness to see how severe your heart failure is.
HF-rEF. If you have an EF of less than 35%, you have a greater risk of life-threatening irregular heartbeats that can cause sudden cardiac arrest/death. If your EF is below 35%, your doctor may talk to you about treatment with an implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy (CRT). Your doctor may also recommend specific medications or other treatments, depending on how advanced your heart failure is. Less common treatment options include a heart transplant or a ventricular assist device (VAD). If your quality of life is very poor or your doctor has told you that your condition is very severe, please ask about other possible treatments.
Some patients have HF-rEF (and an EF lower than 40%) and signs of HF-pEF, such as a stiff (but not always enlarged) left ventricle.
What are the symptoms of heart failure?
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn't mean you no longer have heart failure. Symptoms of heart failure can range from mild to severe, and may come and go.
In general, heart failure gets worse over time. As it worsens, you may have more or different signs or symptoms. It is important to let your doctor know if you have new symptoms or if your symptoms get worse.
Common signs and symptoms of heart failure
- Shortness of breath or trouble breathing. You may have trouble breathing when you exercise, or when you rest or lie flat in bed. Shortness of breath happens when fluid backs up into the lungs (congestion) or when your body isn't getting enough oxygen-rich blood. If you wake up suddenly at night to sit up and catch your breath, the problem is severe and you need medical treatment.
- Feeling tired (fatigue) and leg weakness when you are active. When your heart does not pump enough oxygen-rich blood to major organs and muscles, you become tired and your legs may feel weak.
- Swelling in your ankles, legs and abdomen; weight gain. When your kidneys don't filter enough blood, your body holds onto extra fluid and water. Extra fluid in your body causes swelling edema and weight gain.
- Need to urinate while resting at night. Gravity causes more blood flow to the kidneys when you are lying down. So, your kidneys make more urine and you have the need to urinate.
- Dizziness , confusion, difficulty concentrating, fainting. You may have these symptoms because your heart isn't pumping enough oxygen-rich blood to the brain.
- Rapid or irregular heartbeats (palpitations): When your heart muscle does not pump with enough force, your heart may beat faster to try to get enough oxygen-rich blood to major organs and muscles. You may also have an irregular heartbeat if your heart is larger than normal (after a heart attack or due to abnormal levels of potassium in your blood).
- A dry, hacking cough. A cough caused by heart failure is more likely to happen when you are lying flat and have extra fluid in your lungs.
- A full (bloated) or hard stomach, loss of appetite or upset stomach (nausea).
It is very important for you to manage your other health conditions, such as diabetes, kidney disease, anemia, high blood pressure, thyroid disease and asthma or chronic lung disease. Some conditions have signs and symptoms that are similar to heart failure. If you have new or worsening non-urgent symptoms, tell your healthcare provider.
What causes heart failure?
Heart failure can be caused by many medical conditions that damage the heart muscle. Common conditions are:
- Coronary artery disease (also called coronary atherosclerosis or “hardening of the arteries”) affects the arteries that carry blood and oxygen to the heart (coronary arteries). The normal lining inside the arteries breaks down, the walls of the arteries become thick, and deposits of fat and plaque partially block the flow of blood. Over time, the arteries become very narrow or completely blocked, which causes a heart attack. The blockage keeps the heart from being able to pump enough blood to keep your organs and tissues (including your heart) healthy. When arteries are blocked, you may have chest pain (angina) and other symptoms of heart disease.
- Heart attack. A heart attack happens when a coronary artery suddenly becomes blocked and blood cannot flow to all areas of the heart muscle. The heart muscle becomes permanently damaged and muscle cells may die. Normal heart muscle cells may work harder. The heart may get bigger (HF-rEF) or stiff (HF-pEF).
- Cardiomyopathy. Cardiomyopathy is a term that describes damage to and enlargement of the heart muscle not caused by problems with the coronary arteries or blood flow. Cardiomyopathy can occur due to many causes, including viruses, alcohol or drug abuse, smoking, genetics and pregnancy (peripartum cardiomyopathy).
- Heart defects present at birth (congenital heart disease).
- Diabetes.
- High blood pressure (hypertension). Blood pressure is the force of blood pushing against the walls of your blood vessels (arteries). If you have high blood pressure, it means the pressure in your arteries is higher than normal. When blood pressure is high, your heart has to pump harder to move blood to the body. This can cause the left ventricle to become thick or stiff, and you can develop HF-pEF. High blood pressure can also cause your coronary arteries to become narrow and lead to coronary artery disease.
- Arrhythmia (abnormal heart rhythms, including atrial fibrillation).
- Kidney disease.
- Obesity (being overweight).
- Tobacco and illicit drug use.
- Medications. Some drugs used to fight cancer (chemotherapy) can lead to heart failure









0 Comments